Childbirth is a wonderful miracle, but it does have its own unique complications, some of which people are hesitant to talk openly about. Regardless of whether you have a vaginal delivery or cesarian section, prolapse is a very real possibility. There are many effective ways to treat prolapse, but first we should talk about why it happens, as well as the different types of prolapse.
Estrogen and progesterone are the primary pregnancy hormones. Estrogen helps with vascularization to the fetus, and stimulates milk production. Progesterone causes laxity (or loosening) of the ligaments and joints throughout the body. This allows the uterus to transform from a small pear into a space that can accommodate a full-term baby. Throughout the pregnancy, this increased laxity plus the weight of a growing baby adds a lot of force or pressure onto the pelvic organs. Then during childbirth, you’ve got pushing and pressure, both of which can cause a additional stretching of the ligaments and fascia. In cases where there’s a very long second stage pushing, this can inflict even more force upon the organs within the pelvis.
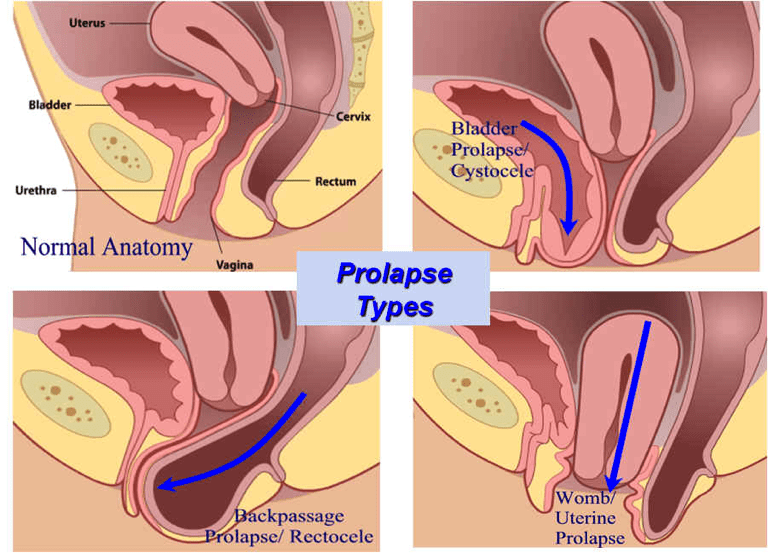
There are three different kinds of prolapse: a cystocele or bladder prolapse, occurs when the bladder falls or presses into the anterior (front) vaginal wall; a rectocele is when the rectum falls or presses into the posterior (back) vaginal wall; a uterine prolapse is when the uterus protrudes into vaginal canal.
How will you know if you have a prolapse?
You may feel some pressure or something hanging down into pelvis. You may also see something protruding out of the vaginal opening. Both of these may indicate that a pelvic floor prolapse is present. To be properly diagnosed, be sure to schedule a follow-up appointment with your OBGYN will be helpful – probably about 6 weeks after you give birth. They will have you bear down or push to observe what occurs. Once diagnosed, there are a few options to consider for treatment: physical therapy, pessary, or surgery.
Pelvic floor physical therapy is the least invasive of treatments. Your physical therapist will do a full evaluation to assess posture, strength, as well as an internal examination of the pelvic floor muscles. The primary goals of treating prolapse will be to reduce any excessive pressure onto the pelvic floor. This will include sharing breathing techniques for having bowel movements, as well as teaching body mechanics and proper lifting techniques.
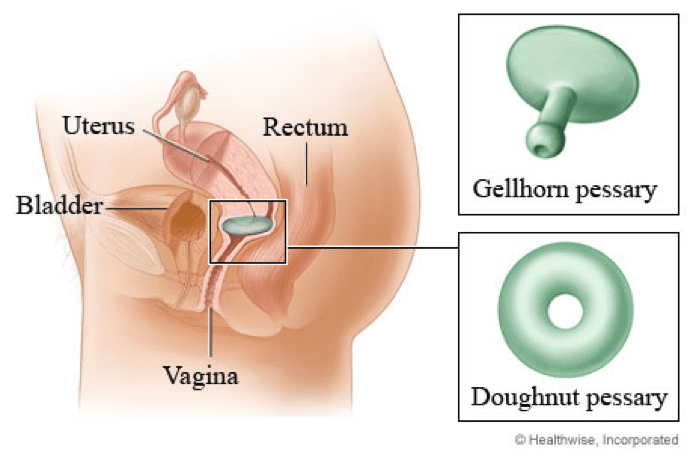
A pessary is a small ring like device, that is inserted vaginally to provide support for for the pelvic floor muscles, and keep the prolapse from hanging down further into the vaginal opening. Your doctor will fit this for you, it may take a few trials to get a good fit. Once you receive the pessary, you will most likely have to change it yourself, but in some cases the doctor can change it every 3 months.
Surgical interventions include: fixation or suspension of the tissues that are loose, either vaginally or abdominally. Usually a mesh is placed when abdominal surgery is performed. With surgery, there could be complications, which could include difficulty urinating and/or incontinence, as well as pain after sex. A hysterectomy can also be performed if the uterus is prolapsed, this can be done vaginally or abdominally.
Usually with time, the prolapse will improve. Once you are finished breastfeeding, your hormones will regulate, therefore reducing the ligamentous laxity. With this regulation of hormones, your pelvis with stabilize and the pelvic floor will be able to work better. If you still have questions about prolapse, follow-up with your doctor and discuss your possible options for treatment.
The Bottom line: If you do have prolapse, please don’t freak out! There are plenty of treatment options, and most likely your prolapse symptoms will decrease. Before you consider surgery, physical therapy is always a great option for basic strengthening and breathing techniques.